How to Manage Gestational Diabetes with Diet and Lifestyle
Pregnancy can be a life-changing experience for many women. There are many highs and lows, happiness and challenges.
To add a diagnosis of Gestational Diabetes Mellitus (GDM) can be very overwhelming.
You may even leave your OB/GYN appointment clueless, with a brand new GDM diagnosis and no explanation of what that means.
Having worked with over 200+ patients with GDM, in this blog, we will break down all things GDM, including diagnosis, risk, and practical nutrition and lifestyle management strategies.
How is Gestational Diabetes Mellitus diagnosed?
Around 24-28 weeks of pregnancy, your OB/GYN sends you for blood work. This includes an oral glucose tolerance test (OGTT), where you drink a very sugary solution and test your blood sugars 1 hour and 2 hours later. If your results come back outside of “normal” targets, then you are diagnosed with gestational diabetes by your OB/GYN.
After a diagnosis, you’ll likely be referred to a diabetes education center (DEC) and have a visit with a dietitian and a nurse (BUT the level of support depends on each DEC location and resources available). You’ll also be followed by an endocrinologist who is a diabetes doctor.
However, until that initial appointment happens, or even after (remember, the level of support varies), you may end up googling “GDM”, and that's probably how you may have ended up here!
What is gestational diabetes?
Gestational diabetes happens during pregnancy when your hormones are changing and likely going a little crazy, causing you to produce less insulin. When you eat food it gets broken down into sugar and enters your blood. Insulin is a hormone that your body produces that acts like a “key” to “unlock the door” to your muscles and cells, allowing sugar to enter from the blood.
When you don’t make enough insulin, the sugars stay in your blood, and when high can cross the placenta into the baby. The baby is smart. It does not need mama’s insulin, so it makes its own and absorbs the extra sugar. But the baby is being “overfed,” and over a long period, this can lead to the baby being bigger than needed.
Remember this is not a reflection of your actions or negligence; rather, GDM is a common condition that happens in pregnancy. Between 3-20% of women will develop GDM at some point in their pregnancy. You are not alone!
Risks of gestational diabetes
Increases rate of C-section
Early (preterm) birth
Increased risk of high blood pressure
Larger than ideal baby size
Increased risk of heart disease and type 2 diabetes in mom and baby later in life
Baby can have a low blood sugar at birth
Very important announcement - just because you have GDM does not mean that your baby will be born with diabetes. Most likely the high blood sugar situation will go away for you after you deliver and your hormones return to pre-pregnancy levels.
Managing gestational diabetes
The good news is that GDM can be managed through diet and lifestyle changes. The first step to managing involves testing your blood sugars.
1. Testing blood sugars:
This is the first and most important step in managing GDM. Your blood sugars have to be in tight control and mostly in the target range so that we are not overfeeding the baby. The only way to know if they're in the target range is by testing. Also, this data is helpful for you to learn if the diet and lifestyle changes you are making are effective.
To get started:
Ask your OB/GYN for a prescription to pick up blood sugar testing supplies (glucometer, testing strips, lancets/needles)
Start testing your blood sugars 4x/day (if you have never tested your blood sugars before and feel overwhelmed and need help, ASK your pharmacist to show you - you pay a dispensing fee they are supposed to help!
Times you need to test:
As soon as you wake up (fasting)
1 hour after breakfast
1 hour after lunch
1 hour after dinner
Your blood sugar target ranges:
Wake up (fasting) between 3.8-5.2 mmol/L
1 hour after the meal should be between 5.5 - 7.7 mmol/L
2. Dietary changes
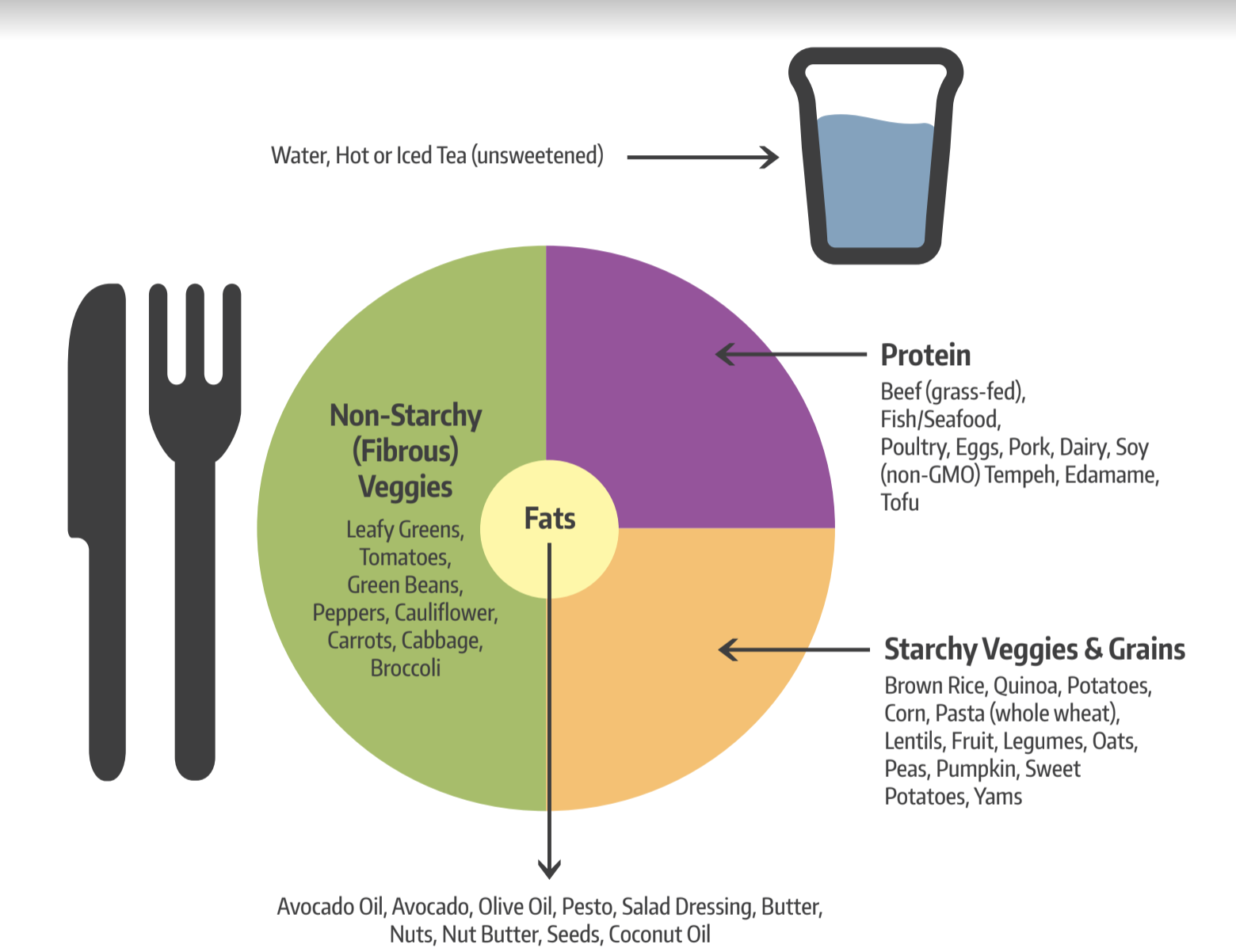
Diet plays a huge role in GDM management. The next time you look down on your plate you’ll notice that some foods turn into sugar while some foods don’t. Foods that turn into sugar are primarily carbohydrates like starches/grains (rice, bread, pasta, roti, potato), dairy products, fruits and sweet vegetables (corn, beets, carrots). Foods that do not turn into sugar are non-starchy proteins and vegetables and healthy fats and oils.
*Note just because a food turns into sugar does not make it bad! You just need to be mindful of your portions and balance with foods that do not turn into sugar. Like see the picture below, try to aim to have:
1/4 of your plate with starches/grain
1/4 of your plate protein
1/2 of your plate with non-starchy vegetables
The key is smaller portions of carbs spread out throughout the day.
What about sweets? We do encourage people with GDM to minimize added sugars, as they’ll likely spike blood sugars. But we don’t want it to feel like your pregnancy is a punishment or foods are off-limits. To occasionally enjoy your favourite sweets, be mindful of frequency and portion, eat it in between meals, consider cutting down on the carb portion at meals, and engage in light walking for 15-20 minutes after (unless medically advised to do otherwise).
Fruits: Despite popular belief, you are okay to eat any fruit that you like! But they do have carbs, so pay attention to how it fits into the rest of your meal. Usually, we recommend spreading fruit out and eating one at a time as a snack.
Snacks: On that note, snacks are a great tool. As you start to reduce or change your portions at meal times you may find yourself getting hungrier. This is a good opportunity to add snacks in between meals. Just remember to wait 1 hour after having your meal to test your blood sugar, and then have your snack.
A simple balanced snack formula we recommend is to have a carb + protein. Here are some examples: fruit + nuts, fruit + Greek yogurt, and fruit + cottage cheese are great examples.
Important note for vegetarians: many plant proteins may be starchy - like lentils, beans, and legumes. We do recommend considering them as your starch or grain (as they contain carbs), so be mindful of your portion. Once again, pay attention to how it fits into the overall balance of your meal!
For personalized nutrition support and meal planning to manage gestational diabetes, work with our Registered Dietitians in our 1-on-1 nutrition coaching programs.
What happens if I try everything and nothing works to bring my blood sugars to the target?
If your blood sugars are consistently above target ranges and diet and lifestyle changes are not helping then you will need to be referred to see an endocrinologist (diabetes doctor). The endocrinologist may start you on medication to help improve your blood sugars. If you need to go on medication to manage your blood sugars it is not a reflection of not trying hard enough or not caring enough. Sometimes despite trying everything due to the hormonal changes, the blood sugar readings might still be above target.
3. Lifestyle strategies to manage GDM
Beyond dietary changes, making lifestyle changes can help in managing gestational diabetes:
Stay Active: Engage in gentle exercises like walking, swimming, or prenatal yoga. Try to do some light walking for 15-20 minutes after meals. Consult your healthcare provider to identify safe and suitable activities that support both you and your baby's well-being
Adequate Sleep: Prioritize getting enough sleep. The demands of growing a tiny human are a lot and rest is important for maintaining stable blood sugar levels.
Stress Management: Explore stress-reducing techniques, such as deep breathing, meditation, or prenatal massages. High-stress levels can impact blood sugar, so finding effective ways to relax is important.
Support System: Surround yourself with a supportive network. Share your experiences, concerns, and triumphs with friends, family, and your healthcare team who can offer guidance and encouragement. Our Registered Dietitians can provide compassionate and evidence-based support to empower you throughout your pregnancy.
Overall, managing gestational diabetes is a holistic approach including dietary adjustments, lifestyle modifications, and a supportive network. Remember, you're not alone in this journey, and with a combination of mindfulness, healthy choices, and gentle self-care, you can navigate through gestational diabetes with confidence. Embrace this transformative time, trust your instincts, and don’t let this hold you down in cherishing your pregnancy!
Hi! I’m Prabhsimran
A Registered Dietitian and reproductive and chronic disease health expert. I’m here to help you gain confidence to overcome your Polycystic Ovary Syndrome and health woes while bettering your relationship with food.
CATEGORIES
Looking for support to help manage your gestational diabetes
Work with our team of Registered Dietitians in 1-on-1 Nutrition Coaching Programs to receive personalized nutrition guidance, meal plans and messaging support to gain knowledge, confidence and clarity to build healthy eating habits that last.
References
Gestational Diabetes. Diabetes Canada
Diabetes and Pregnancy. Diabetes Canada